What Are the Recommended Asthma Treatment Guidelines?
The below content is derived from research done using sources available on the internet. Safey Medical Devices Inc and its subsidiaries do not take any responsibility for the accuracy of the content. No medical decision should be taken on the basis of below content without consulting with your Medical Practitioner.
Late last year, the National Institute of Clinical Excellence (NICE) updated its Asthma treatment guidelines. How is asthma now diagnosed and treated in 2018?
In November 2017, the National Institute of Clinical Excellence (NICE) unveiled new asthma treatment guidelines, as well as revised approaches for the diagnosis of asthma. These amendments are applicable to all NHS-based asthma services throughout England. The new framework is designed to improve the accuracy of asthma diagnosis and revolutionise the types of treatment and monitoring devices capable of keeping the most severe asthma symptoms at bay.
It is hoped the NICE’s new asthma treatment guidelines will give GPs and asthma nurses greater confidence when diagnosing youngsters and adults with asthma. As with all kinds of illnesses and disease, those suffering with asthma require accurate and timely diagnosis so that they can be administered with the best possible medication that can ease day-to-day symptoms and maintain their quality of life.
Guidelines for asthma diagnosis
The most important aspect of asthma diagnosis is being able to sit down with a doctor or nurse that you can trust to discuss your medical history, your family’s long-term history of asthma and any underlying symptoms or triggers that could accelerate the onset of asthma.
The revamped NICE guidelines for asthma diagnosis now state that diagnostic tests are necessary prior to administering any kind of asthma medication or treatment. At the time of writing, there is no definitive asthma diagnostic test for individuals suffering with asthma symptoms.
Instead, there are a range of tests, such as peak flow tests, spirometry and FeNO, which are now stipulated in the NICE guidelines as essential ways of diagnosing and ruling out asthma – prior to the development of any kind of asthma treatment plan.
The guidelines differ somewhat for younger people, particularly those aged five and under with asthma symptoms. In fact, the NICE’s revamped asthma treatment guidelines state that tests such as peak flow and spirometry are inadequate for patients so young. In this instance, GPs are within their rights to implement a “trial of treatment”, combined with close monitoring, to determine the effectiveness of asthma medication.
The diagnostic algorithm used for those who present with respiratory symptoms
In order for GPs and asthma nurses to ascertain whether a patient has a high, intermediate or low probability of asthma, the guidelines now provide a clear algorithm or workflow for medical practitioners to follow.
It starts by assessing an individual’s previous medical records before venturing into tests for airway obstruction, variability and eosinophilic inflammation or atopy. If it transpires following these examinations that a patient’s asthma probability is low, GPs can then investigate or test for other more likely diagnoses. On the flip side, if poor responses are found from the above tests, GPs can then initiate asthma treatments with greater certainty.
Asthma monitoring in adults
The latest asthma treatment guidelines also stipulate that there should be closer monitoring of patients with poor lung function and a history of asthma attacks in the last 12 months.
The guidelines also outline a range of factors that should be monitored and recorded by medical practitioners, including:
- Symptomatic asthma control
- Lung function – measured using spirometry and peak flow testing
- Asthma attacks and time ill since previous assessment
- Inhaler technique and adherence of medication
- Patient reliance on a bronchodilator
- Any active self-management or personal action plan
Self-management and non-pharmacological management
Speaking of self-management of asthma symptoms, the latest asthma treatment guidelines state that asthma sufferers of all ages should be given self-management education and support with writing a personalised asthma action plan.
The guidelines also list a string of effective strategies that have been proven to maintain self-management of asthma symptoms:
- Proactive reminders to prompt routine action plan reviews
- Structured assessments and tests during routine reviews
- Liaison with community-based pharmacists
- Supply of educational resources to assist patients
- Web-based educational resources and monitoring
- Liaison with other community teams
The guidelines also feature three key non-pharmacological tasks that should be adhered to as part of any overarching action plan:
- Educate parents with asthma about the possible dangers of asthma to their children, particularly if the parents are smokers
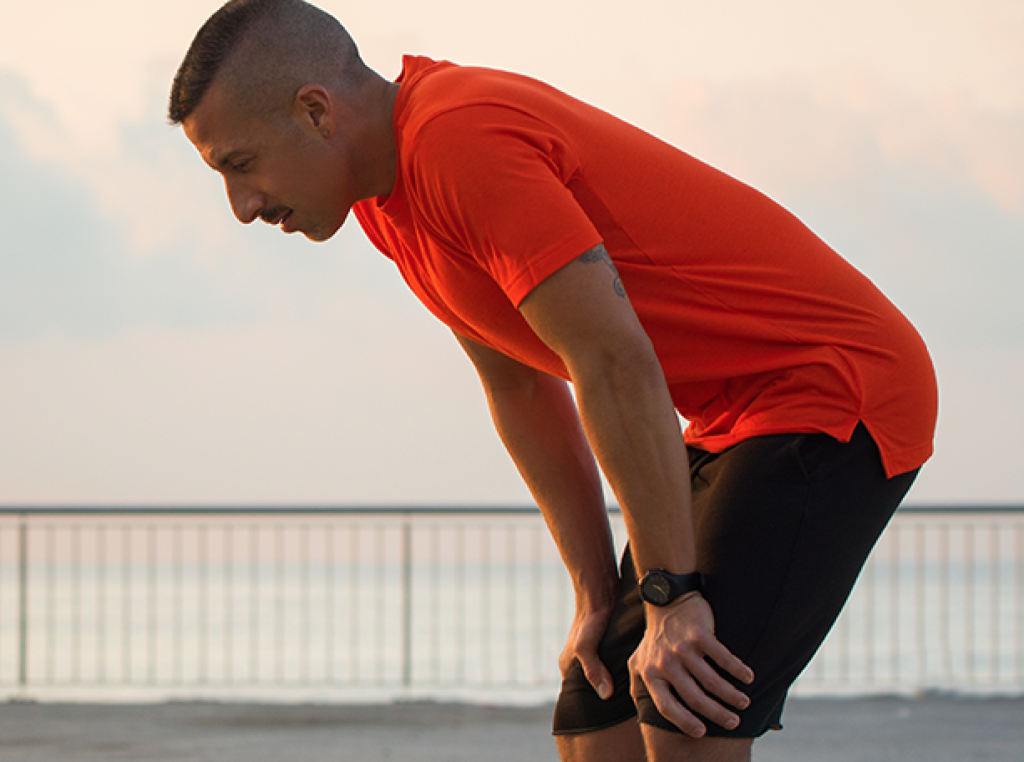
- Interventions to encourage weight loss – through exercise-based and dietary programmes – that help improve asthma control
- Exercises to improve breathing technique and improve quality of life/minimize symptoms of patients
NICE’s asthma treatment guidelines
Traditionally, there have been two types of asthma medication: preventer and reliever medicine. Although this hasn’t changed over the years, the NICE’s asthma treatment guidelines offer a third approach to help asthma sufferers whose symptoms are not resolved through the administering of a steroid-based preventer inhaler.
In the past, these patients would be offered a combination inhaler. The new guidelines state that patients should be offered a tablet, known as a leukotriene receptor antagonist (LTRA). This should be taken simultaneously with the preventer inhaler for up to eight weeks.
However, those who are already using combination inhalers and feel that their asthma symptoms are under control, should not feel the need to alter their asthma treatment.
Inhaler guidelines
The NICE asthma treatment guidelines also discuss the issue of inhaler devices and the technique, training and prescribing of effective devices.
The guidelines state that inhalers should only be prescribed after patients are given necessary training to use the device and that GPs or asthma nurses are satisfied that each patient has an effective technique to administer the medication.
In terms of the prescription of suitable inhaler devices, the guidelines state:
- The choice of a patient’s asthma medication will determine the type of inhaler required
- Patients struggling with their inhaler adherence should be promptly offered an alternative device
- A GP or asthma nurse should assess each patient’s inhaler technique and adherence
- Inhaler technique should be reassessed as part of structured asthma reviews
- Under no circumstances should inhalers be prescribed generically. Asthma sufferers should be given devices they are familiar with
At Safey, we believe our industry leading smart inhaler technology can improve the efficiency of medication adherence among asthma sufferers. Our smart Bluetooth-enabled inhalers not only help you with your inhaler technique, they communicate with caretakers and clinicians to ensure your lungs are receiving the medicine they need to improve your airways.
By controlling your asthma symptoms, we can minimize the economic and emotional burden on the UK’s healthcare system, whilst helping asthma sufferers to lead a normal, happy lifestyle.